Current Suspected Overdose Deaths in Delaware for 2024: Get Help Now!
Find school water testing results and additional resources
Attention Medicaid Participants: Eligibility Renewals Restarted April 1, 2023
Antimicrobial Stewardship refers to a set of coordinated strategies to improve the use of antimicrobial medications, including antibiotics, antivirals, antifungals, and antiparasitics, with the goal of enhancing patient health outcomes, reducing resistance, and decreasing unnecessary costs.
Antibiotic Stewardship encourages healthcare providers to use the right dose and duration of antibiotics to reduce adverse reactions and to achieve the best possible care for the patient. When stewardship is achieved, the spread of infections caused by multidrug-resistant organisms will decrease and it will drastically minimize the likelihood of developing antimicrobial resistance. The misuse of antimicrobials is one of the world’s most pressing public health problems.
The Delaware Division of Public Health (DPH) and the Healthcare-Associated Infections Advisory Committee (HAIAC) support a coordinated statewide program to promote the appropriate use of antibiotics across the healthcare continuum, thus improving patient outcomes and decreasing the spread of multidrug-resistant bacteria.
White House Proclamation on Antibiotic Stewardship
The National Action Plan for Combating Antibiotic-Resistant Bacteria, issued by President Obama on September 18, 2014, provides a road map to guide the nation in rising to this challenge. It outlines steps for implementing the National Strategy for Combating Antibiotic-Resistant Bacteria and addressing the policy recommendations of the President’s Council of Advisors on Science and Technology (PCAST).
Although its primary purpose is to guide activities by the U.S. government, the National Action Plan is also designed to guide actions by public health, health care, and veterinary partners in a common effort to address urgent and serious drug-resistant threats that affect people in the U.S. and around the world. Implementation of the National Action Plan urges action at the national, regional, and local levels to combat resistance.
Antibiotic resistance is a growing problem, and the main cause of this problem is the misuse of antibiotics. CDC’s Get Smart: Know When Antibiotics Work program works to make sure antibiotics are prescribed only when they are needed and used as they should. The Get Smart program focuses on common illnesses that account for most of the antibiotic prescriptions written for children and adults in doctors’ offices and other outpatient settings.
Get Smart: About Antibiotics Use and Resistance
Since their discovery in the 1920s, antibiotics have transformed our ability to treat infections. As antibiotic resistance increases, these lifesaving drugs do not work as well as they once did, and successfully treating common infections  have become more difficult.
have become more difficult.
Get Smart: Know When Antibiotics Work for Patients/Consumers
Common infections, whether caused by bacteria or viruses, are often painful; and can get in the way of our well-being and everyday lives. Many infections do not require antibiotics, but there are other actions you can take to lessen symptoms.
Get Smart: Know When Antibiotics Work for Healthcare Professionals
CDC’s Get Smart program has resources for healthcare professionals working in outpatient and inpatient healthcare settings, as well as community pharmacies. Recommendations for appropriate antibiotic prescribing, including clinical practice guidelines, have been developed to improve outpatient treatment of common infections in children and adults. CDC’s Get Smart: Know When Antibiotics Work program has developed materials that outpatient healthcare professionals can use to educate their patients about when antibiotic treatment is appropriate.
Get Smart: Know When Antibiotics Work for Partners
Working with a wide variety of partners is critical to the success of the Get Smart: Know When Antibiotics Work program. Learn more about what partners are doing to combat antibiotic resistance in their communities and how you can become a partner.
Educational Resources: Antibiotics and Antibiotic Resistance
These educational resources provide information on antibiotics and antibiotic resistance. They are intended for use by educators, healthcare professionals, and consumers.
Antibiotics have transformed the practice of medicine, making once-lethal infections readily treatable.
The core elements of hospital antibiotic stewardship programs cover there 6 important areas:
The Core Elements Of Antibiotic Stewardship for Nursing Homes adapts the CDC Core Elements of Hospital Antibiotic Stewardship into practical ways to initiate or expand antibiotic stewardship activities in nursing homes. Nursing homes are encouraged to work in a step-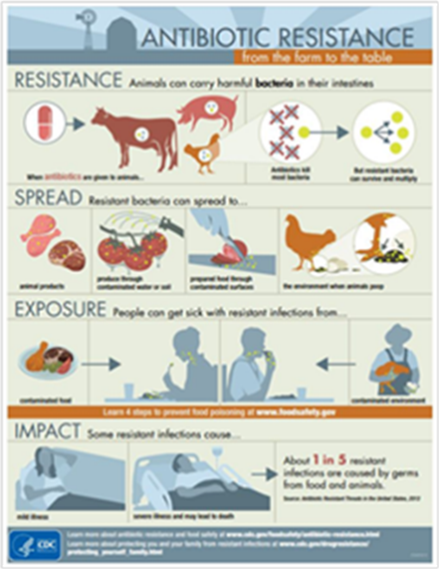 wise fashion, implementing one or two activities to start and gradually adding new strategies from each element over time. Any action taken to improve antibiotic use is expected to reduce adverse events, prevent emergence or resistance, and lead to better outcomes for residents in this setting.
wise fashion, implementing one or two activities to start and gradually adding new strategies from each element over time. Any action taken to improve antibiotic use is expected to reduce adverse events, prevent emergence or resistance, and lead to better outcomes for residents in this setting.
Growth Promotion – The use of some antibiotics can destroy certain bacteria in the gut and help livestock and poultry convert feed to muscle more quickly causing more rapid growth. This class of use has been the subject of controversy and scrutiny, and in 2012, the FDA asked livestock and poultry producers to phase out the use of antibiotics for growth purposes.
Farm to Table
Animals can carry harmful bacteria in their intestines. When antibiotics are given to animals, antibiotics kill most bacteria, resulting in resistant bacteria that can survive and multiply.
State of Delaware, Delaware Health and Social Services, Division of Public Health
Healthcare-Associated Infections (HAIs) are infections that a person acquires while being treated in a healthcare facility, such as a hospital, rehab, or nursing home. HAIs are common and can be painful and sometimes deadly. The Division of Public Health (DPH) works to reduce the number of HAIs, by encouraging prevention methods, such as handwashing, and antibiotic stewardship. To learn more about this topic and their collaboration with national organizations please visit the HAI webpage.
The SHEA Antimicrobial Stewardship Toolkit is comprised of three sections:
Office of Infectious Disease Epidemiology
24/7 Emergency Contact Number: 1-888-295-5156