Trends in Cancer Screening PrevalenceRelatively Steady Among Delaware Adults
There are five major types of cancer which have methods for early detection: breast, cervical, colorectal, lung, and prostate. Of these cancers, the Behavioral Risk Factor Survey (BRFS) collects data on compliance to national recommendations for breast, cervical, colorectal, and prostate cancer screenings. These data are collected in even-numbered years. Beginning in 2018, the BRFS began collecting data on lung cancer screening. This estimate is a point-in-time and trendlines cannot be established.
[Technical Note: Weighting is a process in which a sample is proportionally adjusted to the known population, in this case the adult Delaware resident population. In 2011, there was a major change to the weighting methodology where the number of demographic variables was increased and also allowed the sample to contain both cell phones and landlines. As such, the new methodology increased the validity of the estimates. However, because the change in the new weighting methodology (also knownas raking) was so different, all trendlines prior to 2011 must be broken. To illustrate the change in the broken trendlines, a dark dashed vertical line at 2011 is used for demarcation. Additionally, all trendlines are dashed between 2010 and 2012.]
Any changes observed in prevalence between 2010 and 2012 may be due to the methodology change and not due to an actual change in prevalence of cancer screening.
The Association Between Health Care Access and Cancer Screening
Cancer screenings help detect cancer early. Early detection can lead to better cancer outcomes by reducing late-stage incidence rates and mortality. The BRFS asks questions about clinical breast exams, mammography, sigmoidoscopy and colonoscopy, and prostate-specific antigen. For that reason, health care access, health care coverage, and cancer screenings are covered in this section.
Access to health care is an important factor in cancer screening. The BRFS asked three separate questions regarding access to health care from 2008-2018. The questions included health care coverage status, personal doctor status, and check-up timeliness. The figure below shows the flow of association from access to health care to cancer screening to cancer outcomes.
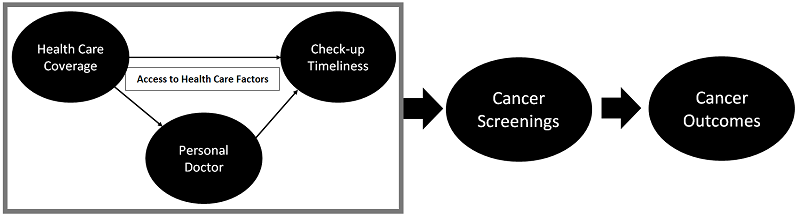 Flow of Association of Health Care Access to Cancer Screening and Outcomes in Delaware
Flow of Association of Health Care Access to Cancer Screening and Outcomes in Delaware
Source: Delaware Health and Social Services, Division of Public Health, Behavioral Risk Factor Survey (BRFS), 2008-2018
Those who do not have access or have poor access are less likely to receive a timely cancer screening, which in turn can lead to increased risk of negative cancer outcomes from diagnosis at a later stage.
Health care coverage (also known as having health insurance) is associated both with having a personal doctor and with having a check-up within the past year. Having a personal doctor does not affect health insurance status.
The “personal doctor” variable is downstream from health care coverage. In other words, having a personal doctor does not affect health coverage status (having health insurance or not having health insurance). Personal doctor is upstream from check-up timeliness. Having a personal doctor is independently associated with having a check-up within the past year.
In contrast, having a personal doctor is associated with having a check-up within the past year. Receiving a check-up does not have any bearing on a person’s health care coverage or personal doctor. However, check-up timeliness is strongly associated with receiving timely cancer screening.
Breast Cancer Screening
Mammogram
The United States Preventive Services Task Force (USPSTF) recommends that all females 40 years of age and older receive an annual mammogram or as recommended by their doctor or health professional. The Delaware Cancer Consortium recommends the same guidelines for breast cancer screening.
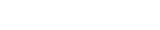
PERCENT OF FEMALES 40 YEARS OF AGE AND OLDER WHO RECEIVED A MAMMOGRAM WITHIN THE PAST TWO YEARS IN DELAWARE, 2008-2018
Source: Delaware Health & Social Services, Division of Public Health, Behavioral Risk Factor Survey (BRFS), 2008-2018.
The prevalence of having received a mammogram among Delaware females 40 years of age and older decreased from 82 percent in 2008 to 79 percent in 2018. However, this decrease is not statistically significant.
There are a number of demographic and access to health care factors captured within the Behavioral Risk Factor Survey. Demographic variables include age, race/ethnicity, educational level, income, and disability status. Access to health care factors include health care coverage, personal doctor, and check-up timeliness. Of all these variables, only two variables (age group and check-up timeliness) were associated with receiving a mammogram within recommendations:
- Females 50-64 years of age were more likely to have received a mammogram within the past two years compared to females 40-49 years of age.
- Females who received a check-up within the past year were more likely to also have received a mammogram within the past two years compared to females who had not received a check-up within the past year.
- Females without a disability were more likely to also have received a mammogram within the past two years compared to females who have a disability.
Cervical Cancer Screening
Cervical cancer screening can be done by two methods: Human Papilloma Virus (HPV) test, and Pap test. The HPV test looks specifically for HPV, a virus known to cause cervical cancers. The Pap test looks for cell changes on the cervix, which could potentially become cancers if not treated appropriately. The United States Preventive Services Task Force (USPSTF) recommends all women between the ages of 21 and 65 receive a Pap test once every three years. A woman between the ages of 30 and 65 can opt to have a HPV test alone or in combination with a Pap test every five years.
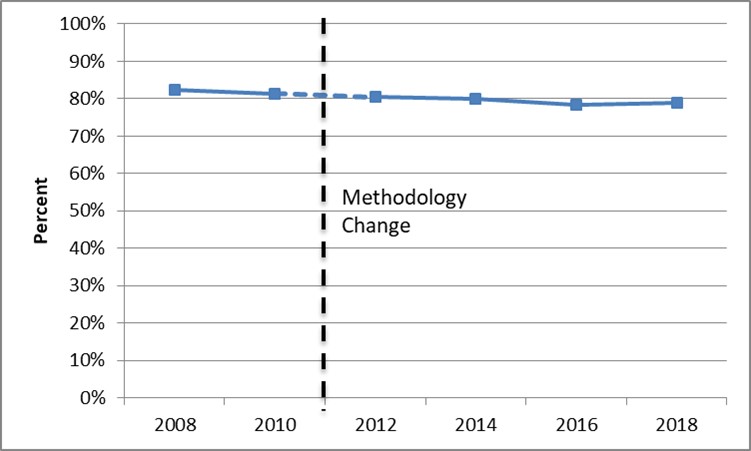
PERCENT OF FEMALES AGE 21-65 WHO HAVE RECEIVED A PAP TEST WITHIN THE PAST THREE YEARS IN DELAWARE, 2008-2018
Source: Delaware Health & Social Services, Division of Public Health, Behavioral Risk Factor Survey (BRFS), 2008-2016.
The prevalence of Delaware females age 21-65 who have received a Pap test within the past three years has declined from a high of 90.1 percent in 2008 to 83 percent in 2018. This decrease is not statistically significant.
Of all the demographic and health care variables, only two variables – an annual household income of $50,000 or more, and receiving a check-up within the past two years – were associated with receiving a Pap test within recommendations:
- Females age 30-65 were more likely to have received a Pap test within the past three years compared to females age 21-19.
- Females with an annual household income of $50,000 or more were more likely to have received a Pap test within the past three years compared to females who had an annual household income of less than $50,000.
- Females who received a check-up within the past two years were more likely to also have received a Pap test within the past three years compared to females who had not received a check-up within the past year.
Colorectal Cancer Screening
There are several methods available to screen for colorectal cancer. These tests include stool tests, flexible sigmoidoscopy, colonoscopy, and CT colonography.
For the stool tests, both the guaiac-based fecal occult blood test (gFOBT) and the fecal immunochemical test (FIT) are used to detect blood in the stool and should be done about once a year. The other stool test, the FIT-DNA test, combines the FIT with a method to detect altered DNA in the stool. The FIT-DNA test can be done every one to three years.
Flexible sigmoidoscopy and colonoscopy are similar tests. Both tests require the insertion of a flexible, lighted tube into the colon to check for polyps or cancer. In the flexible sigmoidoscopy, only the lower third of the colon is checked. During a colonoscopy, the entire colon is examined for polyps or cancer. These tests are recommended once every five years—or every ten years if combined with an annual FIT. CT colonography uses combined images from a CT scanner and X-rays to create a computerized 3-D picture of the colon.
While there are multiple colorectal cancer screening tests available, the United States Preventive Services Task Force (USPSTF) states “colonoscopy is generally considered the criterion standard for test characteristic studies.” In other words, colonoscopy is still seen as the “gold standard” for colorectal cancer screening. Therefore, the Delaware Cancer Consortium recommends that all adults age 50 and older receive a colonoscopy at least every 10 years, or as recommended by their doctor or health professional.
USPSTF Colorectal Cancer Recommendations
Since 2014, the BRFS has asked a series of questions aimed at determining the prevalance of Delaware adults who fully met the USPSTF colorectal screening recommendations.
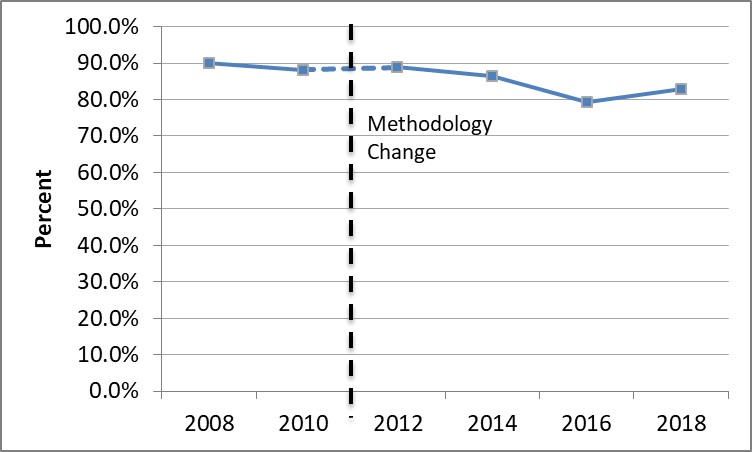
Percent of adults who have fully met the USPSTF recommendations in Delaware, 2014-2018
Source: Delaware Health & Social Services, Division of Public Health, Behavioral Risk Factor Survey (BRFS), 2008-2018.
The prevalence of fully meeting the USPSTF colorectal cancer screening recommendations among Delaware adults has remained stable, from 71.7 percent in 2014 to 73.0 percent in 2018.
Among the demographic and health care variables, only age ground and check-up timeliness variables were associated with fully meeting the USPSTF colorectal cancer screening recommendations.
- Adults age 65 and older were more likely to fully meet the USPSTF colorectal cancer screening recommendations compared to adults age 50-64.
- Adults who received a check-up within the past year were more likely to fully meet the USPSTF colorectal cancer screening recommendations compared to adults whose last check-up was a year or more ago.
Colonoscopy and Sigmoidoscopy
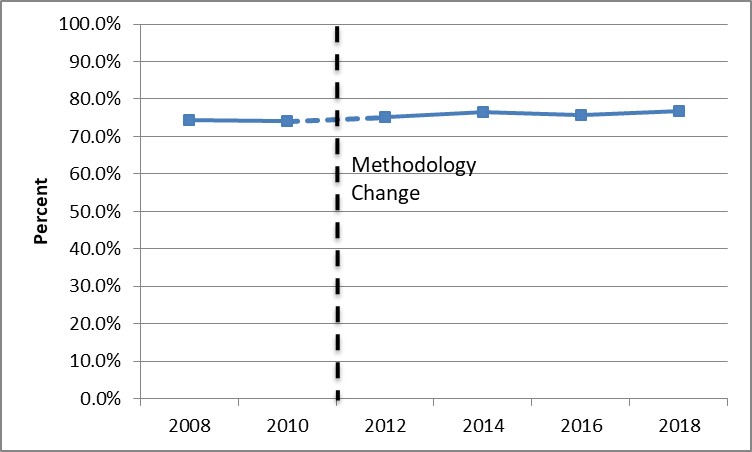
Percent of adults who have ever received a sigmoidoscopy or colonoscopy in Delaware, 2008-2018
Source: Delaware Health and Social Services, Division of Public Health, Behavioral Risk Factor Survey (BRFS), 2008-2018
The prevalence of ever having a colonoscopy/sigmoidoscopy among Delaware adults age 50 and older has remained stable, from 74.3 percent in 2008 to 76.7 percent in 2018.
Among the demographic and health care variables, only age group, check-up timeliness, and personal doctor variables were associated with receiving a sigmoidoscopy or colonoscopy.
- Adults age 65 and older were more likely to ever have received a sigmoidoscopy or colonoscopy compared to adults age 50-64.
- Adults who had a personal doctor were more likely to have received a sigmoidoscopy or colonoscopy compared to adults who did not have a personal doctor.
- Adults who received a check-up within the past year were more likely to have a sigmoidoscopy or compared to adults whose last check-up was a year or more ago.
Prostate Cancer Screening
Screening for prostate cancer is performed by determining the levels of prostate-specific antigen (PSA) in the blood. Prostate-specific antigen (PSA) is a protein produced by both normal and cancerous prostate gland cells. Because there are specific risk factors such as race/ethnicity and family history associated with the incidence of prostate cancer, recommendatons are tiered based on risk category. According to HealthyDelaware.org
- Men who are of average risk should begin screening for prostate cancer at age 0.
- Men who are determined to be high risk shold begin screening at age 45. High risk classification includes African Americans and men who have a first degree relatie diagnosed with prostate cancer before the age of 65.
- Men who are higher risk should begin screening for prostate cancer at age 40. This category includes men who have more than one first-deree relative who had prostate cancer befothe afe of 65.
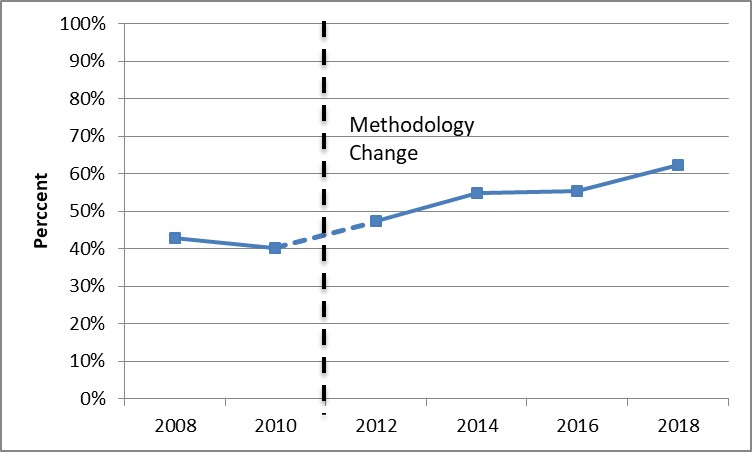
Percent of males who have NOT received a PSA test in Delaware, 2008-2018
Source: Delaware Health & Social Services, Division of Public Health, Behavioral Risk Factor Survey (BRFS), 2008-2018.
The prevalence of NOT receiving a PSA test in the past two years among Delaware adult males age 40 and older increased from 42.9 percent in 2008 to 62.3 percent in 2018. This change is statistically significant.
Of the demographic and health care variables, only check-up timeliness and age group were associated with not having received a PSA test within the past two years.
- Males ages 40-49 were more likely NOT to have received a PSA test within the past two years compared to males age 65 and older.
- Men ages 50-64 were more likely to NOT have received a PSA test within the past two years compaed to males age 65 and older.
- Males whose last check-up was more than one year ago were more likely NOT to have received a PSA test compared to males whose last check-up was within the past year.
- Men should discuss prostate cancer screening with their health care provider before being screened.
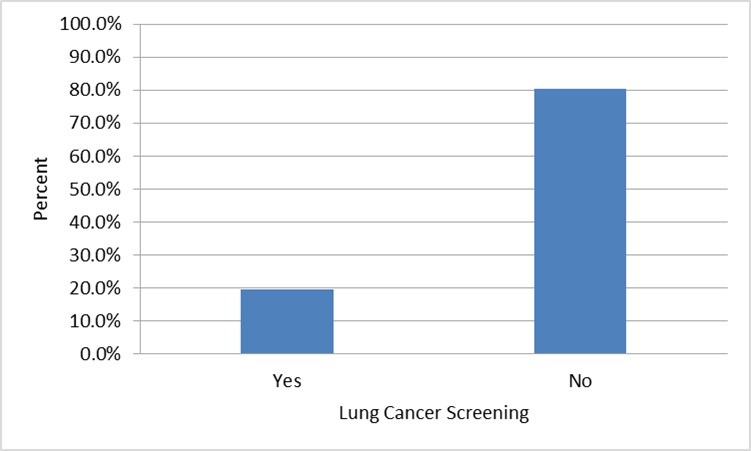
Lung Cancer Screening
“The USPSTF” recommends annual screening for lung cancer with low-dose computed tomography (LDCT) in adults aged 55 to 80 years who have a 30 pack-year smoking history and currently smoke or have quit smoking within the past 15 years.” In 2018, the BRFS began asking questions to determine the prevalence of Delaware adults who are eligible for lung cancer screening and the prevalence of Delaware adults who have had a lung cancer screening. Because this is the first year these questions have been included, these data are only a point-in-time and trendlines cannot be established.
Percent of Delaware adults eligible for lung cancer screening by screening acceptance, 2018
Source: Delaware Health and Social Services, Behavioral Risk Factor Survey (BRFS), 2018
Approximately 11 percent of Delaware adults age 55 to 80 meet the USPSTF eligibility criteria for lung cancer screening. Of those who are eligible, only 19.7 percent report having had a CT or CAT scan for lung cancer screening within the past 12 months. In addition, another 8.6 percent of Delaware adults age 55 to 80 who did not meet the USPSTF eligibility criteria for lung cancer screening reported having a CT or CAT scan within the past 12 months.
Of those Delaware adults who meet eligibility criteria but have NOT received a lung cancer screening with in the past 12 months:
- 55.2 percent are age 55-64
- 51.6 percent are male
- 85.9 percent are non-Hispanic Caucasian
- 55.0 percent have a high school degree or less and 26.2 percent have some college or technical schooling.
- 70.9 percent have an annual household income of less than $50,000